I Found “High Microalbumin” in My Lab Results — and It Felt Like a Punch to the Gut 😰💔
One moment I was living my life, checking blood sugar, trying to eat “healthy.” The next, my doctor said, “Your urine test shows elevated albumin.” My eGFR was still in the 90s (normal), but this microalbumin — this tiny leak of protein into my urine — was a flashing red light: my kidneys were under stress. I left the office with a hollow feeling and a pile of questions. 😢 PMC+1
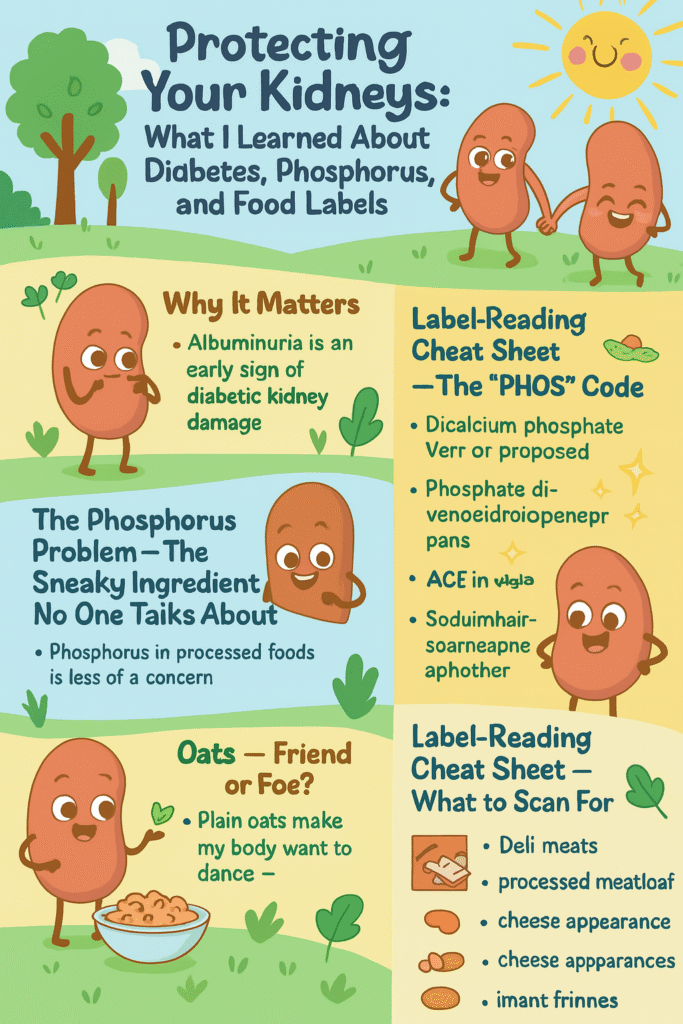
Why this matters: albuminuria (microalbumin) is often the earliest sign that diabetes is starting to damage the kidneys — long before eGFR falls. It’s not something to ignore just because “creatinine looks fine.” Early detection is the moment you can actually do something about progression. PMC+1
The Phosphorus Thing — Quiet, Hidden, and Dangerous (Especially the Added Kind) ⚠️🥫
I’d heard about salt, sugar, potassium. Phosphorus? Not really — until I dug in. Here’s the brutal truth: phosphorus in processed foods (inorganic phosphate additives) is absorbed by your body far more completely than the phosphorus that occurs naturally in whole foods. Studies and reviews repeatedly show that phosphate additives are absorbed at ~80–100% (often near 100%) while much of the phosphorus in plant foods is not fully absorbed (often ~40–60%). That difference matters for people with kidney stress because your kidneys clear phosphorus — and extra absorbed phosphorus forces them to work harder. PMC+1
Worse: phosphate additives are everywhere in processed food — they’re cheap stabilizers, preservatives, texture agents, and they often don’t jump out on the label unless you know what to look for. National Kidney Foundation+1
The Pantry Moment — I Checked My Cabinets and Felt Betrayed 😡🥺
I tore through my pantry. Crackers. Dressed-up cereals. Packaged chicken. Even items I thought were “healthy.” Almost every processed item had a phosphate-related ingredient. My stomach dropped. I realized the problem isn’t just sugar or salt — it’s these invisible phosphate additives that your body soaks up and your kidneys have to deal with. You’re not being dramatic; many people are quietly consuming extra phosphorus without knowing it. JRN Journal+1
What to watch for on ingredient lists: look for “PHOS” or words like dicalcium phosphate, disodium phosphate, monosodium phosphate, phosphoric acid, sodium hexametaphosphate, trisodium phosphate, sodium tripolyphosphate, tetrasodium pyrophosphate. If you see “phos” in the word — be suspicious. National Kidney Foundation
Oats — Friend or Foe? (Short Answer: Mostly Friend — If Plain) 🥣❤️
Oats do contain phosphorus: a typical cooked oatmeal serving often contains roughly ~150–200 mg phosphorus per cup (numbers vary by serving size and brand). But the phosphorus in oats is mostly plant-based (organic) and is less completely absorbed by humans than inorganic phosphate additives. That means plain oats are usually a reasonable, even helpful, choice for people with diabetes and early kidney stress — they bring fiber, slow glucose rises, and support heart health. The real problem is processed oat products (instant flavored packs, fortified cereals, bars) which can include phosphate additives or added sodium/sugars. My Food Data+1
The Science Box — Quick Facts to Drop on Anyone Who Says “Just Eat Anything Whole” 📚🔬
- Albuminuria (microalbumin) is an early and reliable sign of kidney damage and should be confirmed and monitored. Two out of three samples over time are often used to confirm persistent albuminuria. PMC
- Phosphate additives (the chemical kind) are absorbed at ~80–100%, while phosphorus from plant foods and many organic sources is absorbed more slowly and incompletely (often ~40–70%). This makes added phosphates uniquely risky. PMC+1
- Many processed & convenience foods are the main source of added phosphorus — think colas, processed meats, “phosphate-enhanced” chicken, packaged cheeses, deli meats, many fast foods, and some bakery items. DaVita+1
- Blood sugar control is the #1 driver for preventing kidney disease progression in diabetes — controlling A1c and working with your clinician matters even more than obsessing over a single food. Medications and blood pressure control (and sometimes ACEi/ARB therapy) play critical roles in reducing albuminuria — so talk to your doc. KDIGO+1
Real Practical Steps I Took (Doable, Not Perfect) ✅🫶
- I re-committed to blood sugar control. This is the single most protective thing for diabetic kidneys. Talk to your care team about A1c targets and meds. KDIGO
- I read every ingredient panel and learned the “PHOS” code. If something had a suspicious phosphate word, I stopped buying it. Simple. National Kidney Foundation
- I swapped flavored instant oat packets for plain rolled oats and used fruit/nuts for flavor if I needed it. Plain oats < packaged sweetened cereals. My Food Data
- I reduced fast food and ready-to-eat meals. If you can’t cook, choose plain, minimally processed options and ask about ingredients. JRN Journal
- I worked on sodium control (because blood pressure and albuminuria are linked) and focused on whole foods: veggies, controlled portions of lean protein, and fiber. National Kidney Foundation+1
Label-Reading Cheatsheet — What to Scan For (Short & Sharp) 👀📝
Look for any “phos” in the ingredients:
dicalcium phosphate, disodium phosphate, monosodium phosphate, phosphoric acid, sodium hexametaphosphate, trisodium phosphate, sodium tripolyphosphate, tetrasodium pyrophosphate. If it’s there, that food is delivering a highly absorbed form of phosphorus. National Kidney Foundation
Common culprits: cola/soda, processed and deli meats, many cheeses, enhanced/“phosphate-treated” chicken, powdered/instant mixes, many baked goods, and some restaurant foods. DaVita+1
Emotional Reality Check — This Is Scary, But Not Hopeless ❤️🩹🌱
I won’t sugarcoat it: discovering this felt like betrayal — by food, by labels, by my own ignorance. I cried. I was angry. 😭😡 But then I got a map: tests to watch (UACR, eGFR), a list of ingredients to avoid, and clinical steps to take with my doctor. The fear turned into action.
If you’ve just gotten the same news, I see you. The panic is real. The good news: microalbumin is a warning, not the end of the road. With focused glucose control, blood pressure management, thoughtful food choices (especially avoiding phosphate additives), and regular monitoring, many people slow or stop progression. You don’t have to be perfect — you just need to be consistent. PMC+1
🩺 Early Kidney Protection Checklist
For people with diabetes + high microalbumin but normal eGFR
✅ 1. Tests to Watch
Ask your doctor about these regularly:
- UACR (Urine Albumin-to-Creatinine Ratio) – monitor microalbumin
- eGFR (Estimated Glomerular Filtration Rate) – kidney function
- Serum Creatinine – kidney marker
- Serum Potassium & Phosphorus – watch electrolytes
- Blood Pressure – keep <130/80 mmHg (most guidelines)
- A1c (HbA1c) – glucose control (often <7%, individualized)
✅ 2. Medications & Clinical Questions
- Am I on an ACE inhibitor (lisinopril, etc.) or ARB (losartan, etc.) to protect kidneys?
- Should I consider an SGLT2 inhibitor (Farxiga, Jardiance, etc.) — proven to help kidney outcomes in diabetes?
- Do I need medication adjustments if potassium or phosphorus rise?
- How often should I repeat kidney labs?
✅ 3. Diet: Foods to Avoid 🚫
Check every label for “phos” words:
- Dicalcium phosphate
- Disodium phosphate
- Monosodium phosphate
- Phosphoric acid (colas!)
- Sodium hexametaphosphate
- Trisodium phosphate
- Sodium tripolyphosphate
- Tetrasodium pyrophosphate
Common culprits: 🥤 sodas/colas, 🥓 deli meats, 🍗 phosphate-enhanced chicken, 🧀 processed cheeses, 🍪 packaged baked goods, 🍲 instant mixes, 🍟 fast food.
✅ 4. Diet: Foods That Help 🌱💚
- Whole oats, plain oatmeal (not instant packets)
- Vegetables & fruits (unless potassium restriction needed later)
- Beans & lentils (moderation if phosphorus rises, but plant phosphorus less absorbed)
- Whole grains (brown rice, quinoa, barley)
- Fresh, home-cooked meals — avoid processed and pre-seasoned meats
- Low-sodium swaps — herbs, lemon, garlic instead of salt
✅ 5. Lifestyle Habits 🏃♂️
- Keep blood sugar steady (monitor, meds, consistent meals)
- Keep blood pressure in range
- Move daily (walking, light exercise)
- Stay hydrated (unless fluid restriction later prescribed)
- Quit smoking 🚭
- Limit alcohol 🍷
💡 Bottom Line
Microalbumin = early warning, not a death sentence.
You can slow or stop kidney damage by:
✔️ Controlling sugar & pressure
✔️ Avoiding phosphate additives
✔️ Following up on labs with your doctor
🥦 Stage 4 Kidney Disease Diet: What You Need to Know
Living with stage 4 chronic kidney disease (CKD) is not easy. At this stage, your kidneys are only working at 15–29% of normal function. This means waste and extra fluid build up more quickly, and diet becomes one of the most powerful tools you have to protect your health.
I know it can feel overwhelming, but the right kidney-friendly eating plan — personalized to your age, weight, health history, and labs — can help you feel better, slow the disease, and prepare your body for what’s ahead.
🌍 Why Diet Matters at Stage 4 CKD
- Your kidneys can’t filter waste as well. ⚠️ Toxins like urea, creatinine, and phosphorus can build up.
- Electrolytes can swing out of balance. ⚡ Sodium, potassium, calcium, and phosphorus may go too high or too low.
- The right foods protect your heart, bones, and blood vessels, while wrong foods can speed up decline.
- Your doctor and a renal dietitian should work together with you — diet is not “one size fits all.”
🚨 Symptoms You May Notice in Stage 4 CKD
- Less urine output, swelling in hands/feet 💧
- High blood pressure 💢
- Fatigue, weakness, poor sleep 🛌
- Itchy or dry skin
- Muscle cramps or bone pain
- Irregular heartbeats (from high potassium) ❤️⚡
If you’re experiencing these, tell your nephrologist right away.
🥗 General Nutrition Guidelines
At this stage, you’ll need to protect your kidneys by limiting strain:
- Sodium: Low sodium (<2,000 mg/day) to keep blood pressure down.
- Potassium: Restrict if your labs show high levels (2,000–3,000 mg/day typical).
- Phosphorus: Limit (800–1,000 mg/day). Choose natural sources (plant foods) over phosphate additives in processed foods.
- Protein: Often lowered to 0.6–0.8 g/kg/day — but not eliminated. Too much protein = more kidney stress. Too little = malnutrition. Balance is key.
- Calories: Maintain enough calories to prevent muscle loss. Use healthy carbs and fats.
🛑 Foods to Avoid (or Limit)
- 🚫 Processed meats (bacon, hot dogs, deli meat, sausage)
- 🚫 Fast food (phosphate-loaded fries, fried chicken, burgers)
- 🚫 Canned soups, frozen dinners, salty snacks
- 🚫 Cola & dark sodas (phosphoric acid)
- 🚫 Large servings of red meat (high in protein and phosphorus)
- 🚫 Packaged foods with “phos” additives (check labels carefully!)
✅ Safer Food Swaps
- 🍎 Fruits: apples, pears, grapes, berries (low potassium)
- 🥦 Vegetables: cauliflower, green beans, cucumbers, cabbage
- 🍚 Grains: rice, oats, quinoa, barley
- 🥚 Proteins: chicken breast, fish, egg whites, tofu
- 🧂 Flavor: herbs, garlic, lemon instead of salt
💧 Fluids & Lifestyle — Getting the Balance Right
- Stick to this you can get better!!!!
Your kidneys regulate fluid balance — when they’re weak, that balance becomes delicate. Both too much and too little water can be harmful.
✅ General Guidelines (always individualize with your doctor):
- Don’t assume “more water is better.”
In early kidney disease (Stage 1–2), normal hydration is fine. But in Stage 4 CKD, overhydration can cause swelling, shortness of breath, and high blood pressure. - If your doctor gives you a fluid limit, it usually includes everything that melts or is liquid at room temperature: water, tea, coffee, juice, soup, ice cream, ice cubes, gelatin, etc.
- Common fluid limits: 1,000–1,500 mL per day (about 4–6 cups).
This varies based on urine output, weight changes, and heart function. - Weigh yourself daily. A gain of more than 2–3 pounds in 24 hours may mean fluid buildup.
- Check for swelling (ankles, hands, around eyes). Report it quickly — your doctor may need to adjust diuretics or your limit.
- Avoid drinking out of habit or boredom. Try small sips when thirsty, chew gum, or suck on cold grapes, lemon wedges, or ice chips to moisten your mouth.
- Use smaller cups — visually, it feels like more when portioned wisely.
💦 Signs of Too Much Fluid:
- Puffy face or hands
- Swollen ankles or feet
- Shortness of breath, especially lying flat
- Sudden weight gain
- High blood pressure
💧 Signs of Too Little Fluid:
- Dizziness, dry mouth
- Very dark urine (or little urine output)
- Constipation
- Fatigue
📊 Fact: In advanced CKD, even small fluid imbalances can affect heart rhythm, blood pressure, and oxygen levels. Managing intake precisely improves comfort, reduces hospitalizations, and helps dialysis start later.
🧂 Sodium & Blood Pressure — The Fluid Gatekeeper
Sodium and fluid control go hand in hand. When you eat excess salt, your body retains water to balance it — raising blood pressure and swelling.
✅ Kidney-Protective Sodium Tips:
- Aim for <2,000 mg sodium/day (≈ 1 teaspoon of salt total from all foods).
- Skip salty condiments (soy sauce, ketchup, pickles).
- Avoid restaurant and fast food — a single meal can contain 3–4x your daily sodium limit.
- Read every label: “low-sodium” = <140 mg per serving.
- Flavor with herbs, lemon, vinegar, garlic, pepper, or salt-free blends.
- Cook at home — even simple meals let you control your salt.
📊 Fact: Studies show every 1,000 mg sodium reduction can lower systolic blood pressure by ~3–5 mmHg — a major win for kidney and heart protection.
🏃♂️ Physical Activity — Moving to Protect
Even gentle movement helps control blood pressure, glucose, and weight — three of the biggest kidney stressors.
✅ Safe Movement Goals:
- Aim for at least 30 minutes/day, 5 days per week (walking, cycling, light yoga, swimming).
- If fatigue is an issue, break it into 10-minute sessions.
- Avoid “no pain, no gain” — overexertion raises blood pressure and harms tired kidneys.
- Stretch and move every hour if you sit long periods.
📊 Fact: Consistent moderate exercise can lower albuminuria and improve eGFR trajectory in people with diabetes.
(Ref: Clinical Kidney Journal, 2021.)
🩸 Blood Sugar Control — The Root Protector
In diabetic kidney disease, nothing matters more than steady glucose control.
✅ Real-World Habits:
- Test and track blood sugar regularly (including fasting and post-meal).
- Keep A1c close to target (often <7%, individualized by your clinician).
- Eat balanced meals: fiber + lean protein + complex carbs.
- Avoid skipping meals (causes glucose spikes later).
- Discuss SGLT2 inhibitors (like Farxiga, Jardiance) and GLP-1 agonists (like Ozempic, Trulicity) with your doctor — both classes have kidney-protective benefits in diabetes.
📊 Fact: Every 1% A1c reduction can reduce the risk of kidney failure by up to 37% (UKPDS study).
🩺 Blood Pressure — The Silent Strain
High blood pressure silently damages kidney filters (glomeruli) over years.
✅ Protect by:
- Checking BP at home (morning & night).
- Keeping under 130/80 mmHg (unless your doctor advises differently).
- Taking meds consistently — ACE inhibitors (lisinopril) or ARBs (losartan) both lower albuminuria.
- Reducing sodium, managing stress, and sleeping enough (sleep deprivation raises BP).
📊 Fact: Lowering systolic BP by even 10 mmHg can cut kidney disease progression risk by 20–30%.
🚭 Smoking & Alcohol
Smoking:
- Speeds up kidney decline, worsens blood vessel health, and raises BP.
- Quitting immediately improves circulation and filtration.
📊 Smokers with diabetes progress to kidney failure twice as fast as non-smokers (CDC).
Alcohol:
- Occasional small amounts (e.g., 1 drink occasionally) may be fine in early CKD, but avoid frequent drinking.
- Alcohol can dehydrate you, worsen BP, and interact with meds.
- Discuss with your nephrologist — especially if on ACEi, ARB, or diuretics.
💤 Rest, Stress, and Sleep
Your kidneys don’t just filter while you’re awake — they recover while you rest.
- Aim for 7–8 hours of sleep. Sleep deprivation increases cortisol, BP, and blood sugar.
- Manage stress: chronic stress hormones (cortisol, adrenaline) constrict kidney blood vessels.
- Try mindfulness, prayer, breathing exercises, or quiet time before bed.
- Limit caffeine after 2 p.m. (helps BP and sleep).
📊 Fact: Studies link poor sleep quality with faster CKD progression and higher mortality (National Kidney Foundation, 2023).
🫶 Emotional & Mental Health — The Overlooked Vital Sign
Kidney disease isn’t just physical — it’s emotional. Anxiety, sadness, and fear are real and valid.
But emotional support is treatment, too.
- Join a CKD or diabetes support group (online or local).
- Talk to your care team about stress, depression, or burnout.
- Lean on loved ones — you’re not weak for needing help.
- Celebrate progress, not perfection.
📊 Fact: People who engage in structured support (peer or counseling) have 25–35% better treatment adherence and slower disease progression.
🌤️ Putting It All Together
Kidney protection isn’t one big decision — it’s a series of small, loving ones repeated daily:
- Sip wisely
- Move gently
- Rest deeply
- Eat thoughtfully
- Forgive yourself quickly
You are not your lab results — you are the person who shows up every day to protect your body.
💚 The Kidney Care Compass
7 Core Principles for Living Well with CKD
When I first saw “microalbumin” on my lab sheet, it felt like a death sentence.
But it wasn’t. It was a direction sign — a compass pointing me toward change, healing, and peace.
Whether you’re just starting your kidney health journey or managing Stage 4 CKD, these seven principles can guide you every day.
1️⃣ Control Blood Sugar — The Foundation of Kidney Protection 🩸
Every blood sugar spike leaves a mark. Every stable day heals a little.
Why it matters:
High glucose damages the kidney’s tiny filters (nephrons), making them leak protein.
Do this:
- Track your blood sugar patterns, not just random readings.
- Work toward your individualized A1c goal (often <7%).
- Combine medication, meal balance, and movement.
- Discuss SGLT2 inhibitors or GLP-1 agonists — they can protect kidneys and the heart.
📊 Fact: A 1% drop in A1c can reduce kidney failure risk by up to 37%.
(UKPDS Study, The Lancet)
2️⃣ Manage Blood Pressure — The Silent Protector 🩺
Even small improvements matter. Each heartbeat is a message to your kidneys.
Why it matters:
High BP strains the kidney’s filtering units and accelerates damage.
Do this:
- Keep BP under 130/80 mmHg (unless your doctor says otherwise).
- Use ACE inhibitors (lisinopril) or ARBs (losartan) — proven to reduce albuminuria.
- Limit sodium (<2,000 mg/day).
- Check BP at home — small monitors save lives.
📊 Fact: Lowering BP by 10 mmHg can cut CKD progression by 25–30%.
3️⃣ Eat with Awareness — Know the “PHOS” Code 🍽️
Food can either fight for you or against you.
Why it matters:
Phosphate additives stress your kidneys far more than natural phosphorus.
Do this:
- Read every label. If it says “phos”, skip it.
- Avoid processed meats, colas, cheese sauces, and instant mixes.
- Choose whole foods — plain oats, rice, fruits, veggies, fresh proteins.
📊 Fact: Phosphate additives are absorbed at 80–100%, but natural plant phosphorus is only 40–60% absorbed.
4️⃣ Balance Fluids — Not Too Much, Not Too Little 💧
Kidneys love balance. Flooding or starving them both cause harm.
Why it matters:
Fluid buildup strains the heart, while dehydration thickens the blood and worsens toxins.
Do this:
- Follow your doctor’s daily fluid limit (often 1–1.5 L).
- Include soups, ice, and drinks in your total.
- Weigh daily; report sudden gains.
- Control sodium — it directly controls water retention.
📊 Fact: Just 2–3 lbs of overnight weight gain can mean dangerous fluid retention.
5️⃣ Move Gently, Consistently — Circulation Is Medicine 🏃♀️
Movement sends oxygen to kidneys and muscles — it’s a natural detox.
Why it matters:
Exercise lowers BP, improves insulin sensitivity, and reduces inflammation.
Do this:
- Walk or stretch 30 minutes a day, 5 days a week.
- Break it into small sessions if tired.
- Include resistance bands or light weights if cleared by your doctor.
📊 Fact: Regular moderate activity can reduce albuminuria and improve kidney function.
(Clinical Kidney Journal, 2021)
6️⃣ Rest, Recover, and Release Stress 🌙
Your kidneys heal best when you do.
Why it matters:
Stress hormones (cortisol, adrenaline) constrict kidney blood flow and raise BP.
Sleep restores the filtration rhythm and helps blood sugar stabilize.
Do this:
- Aim for 7–8 hours of quality sleep.
- Avoid caffeine late in the day.
- Try deep breathing, prayer, journaling, or gentle stretching before bed.
📊 Fact: People with good sleep quality have up to 35% slower CKD progression.
(National Kidney Foundation, 2023)
7️⃣ Protect Your Heart — Because Heart & Kidneys Are Twins ❤️
What helps your heart, helps your kidneys — and vice versa.
Why it matters:
Cardiovascular disease is the leading cause of death in CKD. The same arteries that feed your kidneys feed your heart.
Do this:
- Control cholesterol (LDL <100 mg/dL, or as advised).
- Quit smoking.
- Stay active.
- Eat omega-3–rich foods (salmon, flax, walnuts).
- Manage stress and sleep.
📊 Fact: People who quit smoking after CKD diagnosis slow kidney decline by up to 30% within one year.
(CDC, 2022)
🌈 The Big Picture — Hope Lives Here
Kidney disease can be terrifying — but it’s also teachable.
Your kidneys aren’t your enemies. They’re your body’s loyal filters, whispering for help.
Every label you read, every walk you take, every glass of water you measure with care —
those are acts of love, not restriction.
This isn’t about punishment.
It’s about preservation.
It’s about giving your body a chance to heal with you, not against you.
And that is what living well with CKD truly means. 💚
Here’s a clear, deep, and factual explanation of anemia in people with kidney disease, including why it happens, how dialysis affects it, treatment options, and what patients should actually do. This is serious but manageable when handled correctly.
What Is Anemia in Kidney Disease?
Anemia means your blood doesn’t have enough healthy red blood cells or hemoglobin to carry oxygen.
In chronic kidney disease (CKD), anemia is extremely common—especially in stage 3–5 CKD and dialysis patients.
By the time someone reaches end-stage kidney disease (ESRD), over 90% of patients develop anemia.
Why Kidney Disease Causes Anemia (The Core Problem)
Healthy kidneys do more than filter waste. They also produce a hormone called erythropoietin (EPO).
1. Loss of Erythropoietin (EPO)
- EPO tells the bone marrow to make red blood cells
- Damaged kidneys can’t produce enough EPO
- Result: red blood cell production drops
2. Iron Deficiency (Very Common)
People with kidney disease often lose iron due to:
- Blood loss during dialysis
- Frequent blood tests
- Poor absorption of iron
- Chronic inflammation blocking iron use (functional iron deficiency)
3. Shortened Red Blood Cell Lifespan
- Normal RBC lifespan: ~120 days
- In CKD: as low as 60 days
- Uremic toxins damage red blood cells
4. Inflammation
- CKD causes chronic inflammation
- Inflammation suppresses bone marrow and iron use
Symptoms of Anemia in Kidney Disease
Many patients suffer quietly. Common symptoms include:
- Extreme fatigue and weakness
- Shortness of breath
- Dizziness or fainting
- Chest pain
- Cold hands and feet
- Brain fog and poor concentration
- Worsening heart disease
Important: Anemia makes kidney disease outcomes worse and increases the risk of heart failure, stroke, and death if untreated.
Anemia and Dialysis: What Changes?
Hemodialysis
- Blood loss occurs during each session
- Dialysis tubing and filters trap red blood cells
- Frequent needle access increases iron loss
- Inflammation remains high
Peritoneal Dialysis
- Less blood loss than hemodialysis
- Still high risk of anemia due to low EPO and iron deficiency
Dialysis does NOT fix anemia on its own.
Most dialysis patients need active anemia treatment.
How Anemia Is Diagnosed in CKD
Doctors monitor:
- Hemoglobin (Hb) – target usually 10–11.5 g/dL
- Ferritin – iron storage
- Transferrin saturation (TSAT) – usable iron
- B12 and folate levels
- Inflammation markers
Important: Pushing hemoglobin too high is dangerous and increases stroke risk. Balance matters.
Treatment Options (What Actually Works)
1. Iron Therapy (Foundation of Treatment)
Oral Iron
- Often ineffective in CKD
- Poor absorption
- Causes stomach upset
Intravenous (IV) Iron (Preferred)
- Used in dialysis and advanced CKD
- Bypasses absorption problems
- Corrects both absolute and functional iron deficiency
Common IV iron types:
- Iron sucrose
- Ferric gluconate
- Ferric carboxymaltose
2. Erythropoiesis-Stimulating Agents (ESAs)
These drugs replace missing EPO:
- Epoetin alfa
- Darbepoetin alfa
- Methoxy PEG-epoetin beta
They:
- Stimulate bone marrow
- Reduce need for blood transfusions
- Improve energy and quality of life
⚠️ Risks if overused:
- High blood pressure
- Blood clots
- Stroke
- Heart attack
That’s why hemoglobin targets are kept modest.
3. Blood Transfusions (Last Resort)
Used only when:
- Severe anemia
- ESA failure
- Active bleeding
- Emergency situations
Downside:
- Iron overload
- Immune sensitization (can prevent kidney transplant eligibility)
4. New Treatments (Emerging)
HIF-PHD inhibitors (oral medications):
- Help body produce its own EPO
- Improve iron utilization
- Still being monitored for long-term safety
What Patients With Kidney Disease Should Do (Action Steps)
1. Demand Regular Anemia Monitoring
- Hemoglobin
- Iron studies
- Not just “once in a while”
2. Treat Iron First
- ESAs don’t work well without iron
- Ask about IV iron if oral iron fails
3. Do NOT Aim for “Normal” Hemoglobin
- Safer target: 10–11.5 g/dL
- Higher is not better
4. Control Inflammation
- Treat infections promptly
- Manage dialysis adequacy
- Address nutritional deficiencies
5. Nutrition Matters (But Isn’t Enough Alone)
Helpful nutrients:
- Iron (heme sources if allowed)
- Vitamin B12
- Folate
- Adequate protein (as guided by renal dietitian)
Diet alone cannot fix CKD anemia, but it supports treatment.
Why This Matters So Much
Untreated anemia in kidney disease leads to:
- Faster kidney decline
- Heart enlargement and failure
- Reduced ability to work or function
- Lower survival rates
- Poor quality of life
Treating anemia is not optional — it is essential care.



